
What is the difference between osteoarthritis and rheumatoid arthritis?
Wednesday, August 18, 2021
Let's begin by defining a few terms. Arthritis is an umbrella term that describes the inflammation of joints. Osteoarthritis is also known as degenerative joint disease. So, in simple terms, there is no difference between osteoarthritis and degenerative arthritis.
However, there is another form of arthritis called rheumatoid arthritis. Although osteoarthritis and rheumatoid arthritis are both forms of arthritis characterised by similar symptoms, the main difference between them is what causes these symptoms.
Here, we're clearly defining osteoarthritis (or degenerative arthritis) and rheumatoid arthritis, the similarities and differences between them, and how you can treat both osteoarthritis and rheumatoid arthritis.
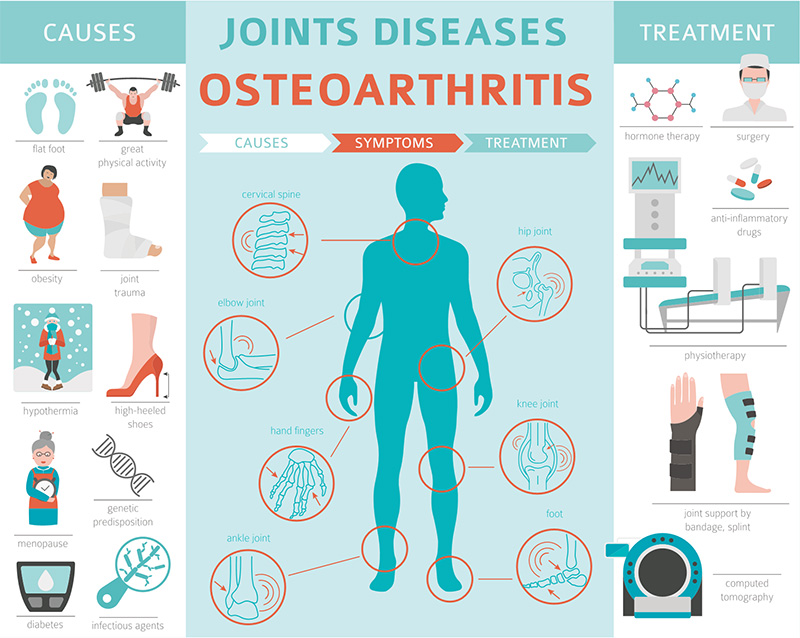
What is osteoarthritis?
Osteoarthritis, or degenerative joint disease, is the most common form of arthritis. It's caused by wear and tear which is why it's commonly associated with the older population. Osteoarthritis usually develops slowly over time as the cartilage between joints gradually breaks down.
Some symptoms of osteoarthritis include tender, achy joints, swelling of the joints, cracking noises coming from your joints as they move, and impaired joint function. Additionally, since osteoarthritis is caused by wear and tear, it often affects some joints more than the other.
For example, we tend to favour one side of our body over the other. For example, right-handed people might experience more osteoarthritis-related joint pain in the right hand than the left. This can occur for many joints throughout the body.
Additionally, since osteoarthritis is caused by wear and tear, our most commonly used joints such as our hips, knees, back, neck, and fingers are often the first joints to feel the effects.
Risk factors for osteoarthritis include:
- Old age
- Overuse of a specific joint
- Obesity or being overweight
- Joint deformities
- Diabetes
- Gout
- Previous traumatic injuries to your joints
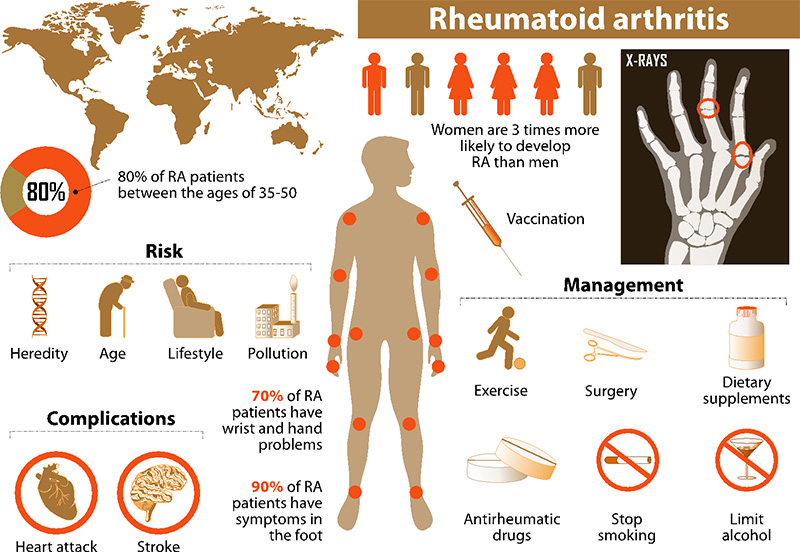
What is rheumatoid arthritis?
As opposed to osteoarthritis, rheumatoid arthritis affects far fewer people than osteoarthritis - only about one-tenth as many. Rheumatoid arthritis has nothing to do with age and is instead due to an autoimmune disease that causes a degeneration of the joints. The body's immune system attacks the tissue of its own joints causing extreme pain and discomfort.
Another characteristic of rheumatoid arthritis that's different from osteoarthritis is that its onset can be rapid, coming on over a period of weeks or months.
Some symptoms of rheumatoid arthritis include extremely stiff, painful, swollen joints. Many who suffer from rheumatoid arthritis also experience extreme fatigue, a poor appetite, lumps called rheumatoid nodules that appear under the skin, and they often feel ill much of the time. These additional symptoms aren't apparent in osteoarthritis.
Since rheumatoid arthritis, again, isn't related to wear and tear, it affects almost every joint in your body, no matter which side, large or small, regardless of how often it's used. However, the onset of rheumatoid arthritis often begins in the smaller joints such as your finger joints.
Plus, rheumatoid arthritis can run in families and be passed down genetically from parent to child, whereas osteoarthritis cannot.
Similarities Between Osteoarthritis and Rheumatoid Arthritis
As you can see, there are many differences between osteoarthritis (degenerative arthritis) and rheumatoid arthritis. However, there are some similarities, too.
First of all, both osteoarthritis and rheumatoid arthritis are more prevalent in females than males. Both forms of arthritis are also more common in older populations but rheumatoid arthritis, as we mentioned, can develop at any age.
The basic symptoms of osteoarthritis and rheumatoid arthritis are also generally the same. Both patients will suffer from sore, stiff joints, warmth or tenderness in the affected areas, and increased sensitivity to their symptoms in the morning.
However, it seems that rheumatoid arthritis is a much more serious condition that can have additional effects such as chronic fatigue and low-grade fevers.
Treatment of Osteoarthritis and Rheumatoid Arthritis
The good news is, there are some ways to treat both osteoarthritis and rheumatoid arthritis. But, with that being said, there's no cure for either type of arthritis and joint damage is irreversible. Instead, the treatment of both osteoarthritis and rheumatoid arthritis focuses on:
- Reducing pain in your joints
- Improving the function of your joints
- Minimising further damage to your joints
- Generally, anti-inflammatory medications and corticosteroids are used to help deal with the inflammation of your joints caused by arthritis. These should also help with the pain associated with both osteoarthritis and rheumatoid arthritis.
When it comes to osteoarthritis, other pain-relieving treatments are often used such as:
- Pain-reducing creams
- Non-steroidal anti-inflammatory drugs
- Pain-relievers like acetaminophen
As always, speak to your doctor before using any medications to treat your osteoarthritis.
Since rheumatoid arthritis is an autoimmune disease, drugs that suppress your immune system can help with treatment. However, these treatment plans come with many caveats and require personalised care. Be sure to speak with your medical doctor about treating your rheumatoid arthritis.
Other Useful Resources
Difference between rheumatoid arthritis and fibromyalgia
How can physiotherapy help osteoarthritis? What you need to know
Osteoarthritis exercises for knee pain
How do I know if I have osteoarthritis or rheumatoid arthritis?
The best way to know whether you have osteoarthritis or rheumatoid arthritis is to consult your doctor. However, some symptoms like symmetry, fever and excessive fatigue can help you tell that you have rheumatoid arthritis versus osteoarthritis. Let's explore these symptoms a bit more.
One symptom of RA that's not always the case with OA is that your joints are likely to feel painful on both sides. So, if your arthritis is symmetrical, you may have RA.
The reason for this symmetry is because RA has nothing to do with wear and tear. It's an autoimmune disease where the cells of your joints are essentially attacking themselves. So, if multiple joints are in pain or both shoulders, both knees or both hips have painful joints, this could be a sign of RA.
On the other hand, OA usually presents itself in an isolated joint. You might feel pain in one hip or in your left knee. Athletes and the ageing population often experience OA due to the fact of overuse, whereas RA can affect people at any age.
Fevers, especially in children are another symptom of RA that you won't find if you have OA.
And additionally, excessive fatigue is also usually present in those with RA that doesn't necessarily occur in those who suffer from OA.
Overall, if you're experiencing joint pain symmetry or pain in more than one joint, you have a fever or you're feeling excessively fatigued, you're more likely to have RA versus OA. But again, it's essential that you speak to a doctor or healthcare professional to be sure.
What is the most painful type of arthritis?
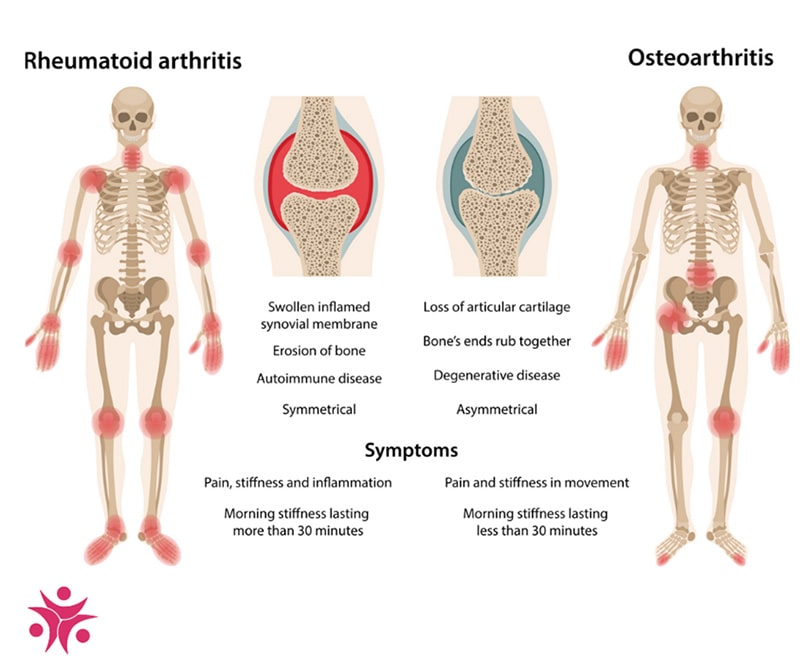
In general, rheumatoid arthritis is more painful than osteoarthritis. RA is more painful for a few reasons including the fact that it presents more symptoms, affects more joints simultaneously and often lasts longer throughout the day.
The most common symptoms of both RA and OA include painful, stiff joints, limited range of motion, warmth and tenderness in affected joints and more intense pain in the morning. However, RA presents additional symptoms apart from OA including fevers, muscle aches and excessive fatigue.
These additional symptoms suggest that RA is more painful since you're experiencing more overall discomfort.
RA also affects more joints than the average case of OA. Since RA is an autoimmune disease that attacks the cells that make up your joints, it often begins in your smaller joints and eventually begins to effects all of the joints of your body.
On the other hand, OA tends only to affect a few isolated joints that are overused or injured. While OA can certainly progress to affect most of your joints, especially as you age, it's estimated that RA is more painful overall since most of your joints will be affected.
And lastly, although both RA and OA symptoms are more intense in the morning before your joints get a chance to loosen up, OA symptoms tend to improve within 30 minutes whereas RA symptoms tend to take longer to feel better. This is a third reason why it's assumed that RA is more painful than OA.
Keep in mind that everybody is different and symptoms present themselves differently from person to person. Depending on the progression and severity, both OA and RA can certainly be painful.
What are the four stages of osteoarthritis?
The four stages of osteoarthritis are 1) minor, 2) mild, 3) moderate and 4) severe.
Stage 1 Minor OA means your joint is showing signs of minor bone spur growth. These bony growths develop near the joint meaning there might be some cartilage loss but, in general, you won't experience much, if any, pain at this stage of OA.
Stage 2 Mild OA reveals greater bone spur growth but the cartilage is still intact, usually within a healthy range and the bones won't be rubbing together. You'll also still usually have normal levels of synovial fluid between your joints at this stage. However, at this point, you'll likely begin to experience some uncomfortable symptoms such as pain after a long period of walking or running, stiffness after the joint hasn't been used in a while and tenderness when bending the joint.
Stage 3 Moderate OA means that your cartilage between the joint has undergone more obvious damage with less space between your bones. You'll likely be experiencing joint pain more regularly especially when walking or bending. You might also start to experience stiffness after long periods of sitting still, some swelling of the joint or more achiness in the morning.
Stage 4 Severe OA means you'll experience intense joint pain and discomfort whenever you move the affected joint due to the space between the bones becoming extremely compromised. The cartilage is completely gone meaning the joint will be stiff and practically immobile with far less synovial fluid to help the joint move properly.
How do you stop osteoarthritis from progressing?
While there's no cure for osteoarthritis, you can slow its progression by reducing inflammation by taking medication and working with a physiotherapist to improve your range of motion and the health of your joints.
Since inflammation is often what's causing the actual pain in your joints due to OA, it makes sense that you can reduce your overall pain while living with OA by taking anti-inflammatory medication as prescribed by your doctor.
However, to improve the overall health of your joints and increase your mobility to continue to live your life as normally as possible, physical therapy is key. You have to move your joints to keep them healthy and by strengthening and stretching the muscles surrounding your joints, they'll become more stable and healthy.
All in all, you won't be able to reverse the onset of OA, but you can stop it from progressing by managing your pain with anti-inflammatories and improving your quality of life through regular physical therapy or physiotherapy.
--
Interested in working with one of our physiotherapists to reduce joint pain, strengthen your body, and even prevent arthritis as much as possible?
Book a consultation and let our mobile services come to you OR alternatively find your local Physio Inq clinic. Arthritis is a painful condition that affects every aspect of your daily life. We'd love to help you toward a more pain-free life. Call Physio Inq today!
This article was originally written by Jonathan Moody from Physio Inq

